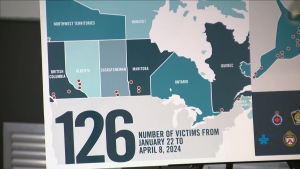
Up to 35 people may die in Ontario in up until early May because their cardiac surgeries were cancelled or deferred to make way for a better response to the COVID-19 pandemic, new research suggests.
“I understand that a report had been released today – by UHN with respect to cardiac deaths and it has been estimated that 35 people may have passed away because their surgeries were not performed,” Ontario Health Minister Christine Elliott said Tuesday, citing research by University Health Network in Toronto. “That’s not something any of us want to hear, it certainly was not intended because the best medical decisions were made.”
The modelling exercise was completed by a group of doctors from multiple Toronto hospitals, and found between 30 to 35 patients waiting for elective but invasive cardiac surgery could die between March 15 and the start of May.
Half of those patients likely to have died during this period were waiting for transcatheter aortic valve implantation, a procedure that thousands across the province were waiting to undergo in March, according to data in the study.
“Compared to the number of potential deaths of COVID-19 patients due to resource depletion under the worst case pandemic epidemiology scenarios, there was only a modest consequence in terms of wait-list morbidity and mortality, at least in the short term for pausing cardiac procedures,” the authors wrote.
In a statement issued later in the day, Minister Elliott's office clarified that the study “does not report on confirmed cases or individuals known to have been impacted.” And that cancelling elective surgeries, “was done operating under the assumption that the province may experience a significant surge in COVID-19 cases, as seen in Italy, Spain and New York, which would have crippled the province’s ability to care for Ontarians.”
Like other specialized hospitals in the province, University Health Network’s Peter Munk Cardiac Care Centre has postponed numerous tests and elective or non-critical surgeries, including certain aortic valve replacements, cardiac tumour removals and myectomies.
But critical surgeries and heart transplants are proceeding as scheduled.
Across the province, the Financial Accountability Office estimates more than 50,000 surgical procedures have been cancelled or postponed to free up hospital space for COVID-19 patients.
“But as I have said before – any death is a tragedy – it’s something that has happened. I don’t want to call it collateral damage because they are deaths,” Elliott said.
Numerous Ontario hospitals were emptied of patients deemed non-critical to make room for a expansion in acute and critical care beds for COVID-19 patients.
As of Tuesday, more than 900 people are in hospital with cases of COVID-19, and 239 are breathing with the help of a ventilator in an ICU.
Ontario Chief Medical Officer Dr. David Williams said he had not read the study yet, but it was never his or Ontario’s COVID-19 Command Table’s intent to have people die while waiting for surgery.
“We did not plan that it would be acceptable to have patients die unnecessarily during this time of delaying elective surgery. It was not in the plan and it would not be acceptable to put that in as a caveat.”
He said that any Ontario doctor in the cardiac field or elsewhere has the freedom to demand their patient receive surgery if their condition worsens to the point that the treatment can no longer be considered elective.
“Nothing stops a physician from saying ‘this needs to be dealt with now’ when it might have been elective two or three weeks ago but now it’s urgent.”
Ford and Elliott have both indicated cardiac and cancer surgeries are at or near the top of the list what they want to resume when emergency measures relax in the next several months.