The number of First Nations people who died from opioid-related deaths in Ontario more than doubled during the first year of the COVID-19 pandemic.
That's one of the key findings of a report released by the Chiefs of Ontario and the Ontario Drug Policy Research Network on Friday, which examined patterns in hospitalizations and deaths due to opioid-related poisoning among First Nations and non-First Nations people in Ontario.
It notes that 116 First Nations people died due to opioid poisoning between March 2020 and March 2021, compared with 50 people in the previous year.
That's a 132 per cent increase, compared to a 68 per cent increase of opioid-related deaths among the rest of the population in the province.
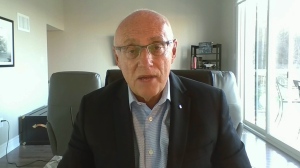
“First Nations have been disproportionately affected by the overdose crisis,” said Ontario Regional Chief Glen Hare in a news release.
“The use of opioids and other substances continues to surge during the COVID-19 pandemic, producing conditions that further increase overdoses and deaths.”
The monthly rate of hospital visits for opioid-related poisoning has increased since March 2016 among both First Nations and non-First Nations people, the report notes.
The number of First Nations people who visited the hospital for an opioid-related poisoning between March 2020 and March 2021 was 816, compared with 601 people in the previous year - marking a 35.8 per cent increase.
In comparison, the number of non-First Nations people who visited the hospital for an opioid-related poisoning increased 16.4 per cent during this period, from 7,441 to 8,662.
The report states the majority of First Nations people who visited the hospital or died due to an opioid-related poisoning lived in urban areas or outside of First Nations communities.
However, during the pandemic, the largest relative increase in opioid-related harms occurred among First Nations people living in rural areas and within First Nations communities. Specifically, just over one in five hospital visits occurred among First Nations people living within First Nations communities between March 2020 and March 2021, compared to one in seven a year prior.
The report also notes that the involvement of fentanyl in opioid-related deaths significantly increased during the pandemic, contributing to 87 per cent of opioid-related deaths among First Nations people and aligning with broader trends across the province.
First Nations people were identified in the report using the Indian Registry System database, which includes people who are eligible for Indian Status under the Indian Act.
The Chiefs of Ontario and the Ontario Drug Policy Research Network also released a report analyzing opioid use, related harms and access to treatment among First Nations in Ontario on Friday.
“The reports released today are very explicit in providing evidence that governments need to correct the underfunding that has been occurring for years to make effective progress on addressing the overdose crisis in First Nations communities,” said Hare.
The Truth and Reconciliation Commission's calls to action urge the federal government to establish measurable goals to identify and close the gaps in health outcomes between Indigenous and non-Indigenous communities.
Hare said many First Nations communities have made “great efforts to strengthen community capacity through community-led programs.”
However, he said the work to implement the recommendations in these reports must expand in order for real progress to happen, to prevent future tragedies and strengthen the healing processes “so desperately needed” in First Nations communities.
“I look forward to meeting with all levels of government immediately to co-ordinate a long-term, First Nations-led strategy to address the opioid crisis affecting First Nations across Ontario,” Hare added.
Ontario's Ministry of Health and Indigenous Services Canada did not immediately provide comment.
This report by The Canadian Press was first published Nov. 26, 2021.
This story was produced with the financial assistance of the Facebook and Canadian Press News Fellowship.