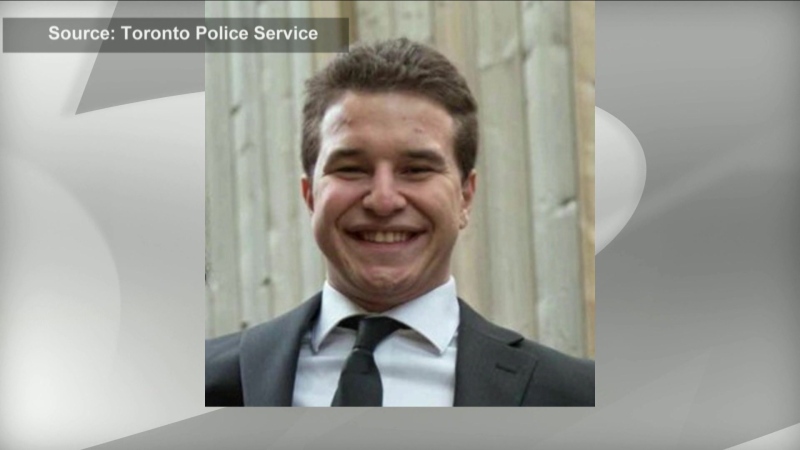
Annalise Mathers doesn't remember the fall that caused her concussion on a ski mountain four months ago, but she can recall the disorienting feelings that followed.
The 28-year-old from Toronto was cut off by a pair of snowboarders while downhill skiing in March, sending her flying awkwardly over a jump and into a patch of snow. While Mathers didn't feel badly hurt when she came to, the headache she developed that night indicated something was amiss.
Mathers was diagnosed with a concussion the following day, marking the beginning of a four-month recovery process full of unknowns, including how her symptoms would manifest and how long they'd last.
“There was this added piece of uncertainty in my life ... not knowing how I would recover, when I would recover,” Mathers said. “You hear such an incredible diverse array of people's own experiences with concussion, and it makes the recovery process really hard to map out.”
Researchers at Toronto's University Health Network are working towards getting some clarity for concussion patients, using data from their recent study to develop a calculator that could help doctors assess who's more at risk for prolonged post-concussion symptoms, or PPCS.
The calculator, ideally used on adult patients when diagnosed, was introduced Thursday by scientists from Toronto Rehab-UHN's KITE Research Institute. It generates risk scores based on patients' answers to five questions.
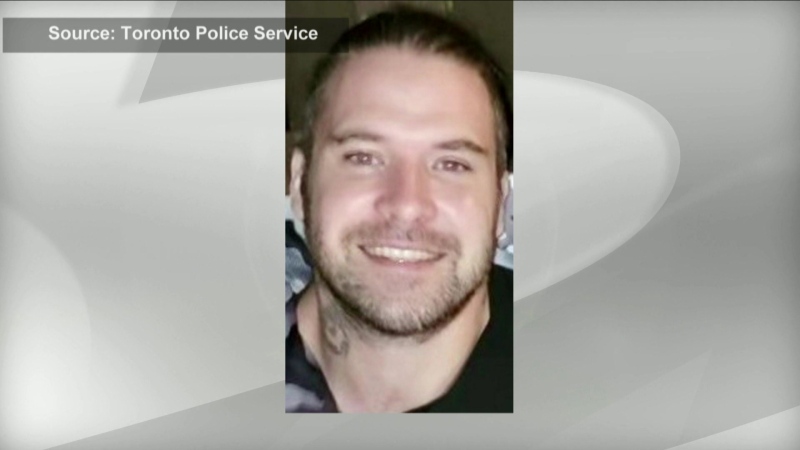
“We thought this might be helpful for clinicians to get this into an easy calculator they could (use) and say, 'OK, does the person in front of me have risk factors for future long-term concussion symptoms?”' said Dr. Mark Bayley, the medical director at Toronto Rehab.
Research from Bayley and others published Thursday in the peer-reviewed journal PLOS Medicine looked at data on past concussion patients in Ontario to identify who needed specialist care at least six months after their concussion.
The team found 12.5 per cent of patients experienced prolonged post-concussion symptoms, though Bayley said the number is likely around 15 per cent when accounting for those who had extended symptoms but didn't seek additional care.
The research suggests people older than 61 years of age and adults with “high levels of health-care usage” in the year before their concussion are higher risk, while those with a history of psychiatric disorders, anxiety or depression are among the highest risk for PPCS.
“When people have pre-existing mental health issues, and then you superimpose on it a concussion, is that making them more vulnerable? Maybe their neurotransmitters are changing ... and we need to pay attention,” Bayley said.
He added that a history of past concussions didn't come up “as strongly as (researchers) thought” for who might develop prolonged symptoms.
PPCS can involve debilitating physical, visual, cognitive and/or emotional symptoms including: headache, dizziness, neck pain, sensitivity to light, concentration problems, absent-mindedness and irritability. Anything that extends past three months post-injury could be considered PPCS, Bayley said.
But what does a high-risk score on the calculator mean for treatment?
Bayley said doctors are still trying to find better ways to help those through PPCS.
“We haven't got that yet, but we believe following them more closely, trying to treat their headaches a bit better, getting them exercising appropriately, having earlier treatment, counselling, relaxation ... could probably result in a reduction in the number of people with long-term symptoms,” he said.
Mathers suffered near-daily headaches with light and sound sensitivity that sometimes prevented her from getting out of bed during the first two-and-a-half months of her concussion.
She said she's at the “end point” of her recovery now, after a treatment plan that focused on symptom management and exercise and support from Toronto's Hull-Ellis Concussion and Research Clinic.
Mathers called that support network a “pillar” of her recovery, especially during the COVID-19 pandemic when social connections were severed.
“I think (the recovery process) can be very isolating, particularly for people who may not know they have a concussion or know the severity of it,” Mathers said. “It ties into the invisible nature of concussions - someone can look at you and not really know why you might be struggling physically and mentally.”
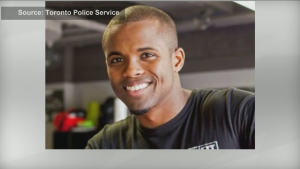
Dr. Alice Kam, a member of the UHN research team who's been using the concussion calculator in her own practice for six months, said it can be frustrating for patients to not know how long their symptoms may last, and frustrating for doctors who don't always have answers to give.
“There are many unknowns with concussions,” Kam said. “So this calculator will be really helpful in terms of helping us triage and provide some reassurance to patients.”
This report by The Canadian Press was first published July 8, 2021.