FORT LAUDERDALE, Fla. (AP) - Florida hospitals slammed with COVID-19 patients are suspending elective surgeries and putting beds in conference rooms, an auditorium and a cafeteria. As of midweek, Mississippi had just six open intensive care beds in the entire state.
Georgia medical centers are turning people away. And in Louisiana, an organ transplant had to be postponed along with other procedures.
“We are seeing a surge like we've not seen before in terms of the patients coming,” Dr. Marc Napp, chief medical officer for Memorial Healthcare System in Hollywood, Florida, said Wednesday. “It's the sheer number coming in at the same time. There are only so many beds, so many doctors, only so many nurses.”
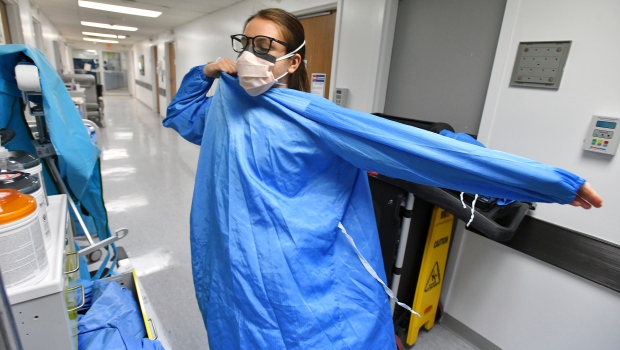
Coronavirus hospitalizations are surging again as the more contagious delta variant rages across the country, forcing medical centers to return to a crisis footing just weeks after many closed their COVID-19 wards and field hospitals and dropped other emergency measures.
The number of people now in the hospital in the U.S. with COVID-19 has almost quadrupled over the past month to nearly 45,000, turning the clock back to early March, according to the Centers for Disease Control and Prevention.
That's still nowhere close to the nearly 124,000 people who were in the hospital at the very peak of the winter surge in January. But health experts say this wave is perhaps more worrying because it has risen more swiftly than prior ones. Also, a disturbingly large share of patients this time are young adults.
And to the frustration of public health experts and front-line medical workers, the vast majority of those now hospitalized are unvaccinated.
Florida, Georgia, Louisiana and Mississippi alone account for more than 40% of all hospitalizations in the country.
Mississippi has one of the lowest vaccination rates in the nation, with less than 35% of its population fully inoculated, and Louisiana and Georgia aren't much better, at around 38%. Florida is closer to the national rate at 49%, but none of the four Southern states comes close to the New England region, where most states are well over 60%.
The variant has sent new U.S. cases surging to 94,000 a day on average, a level not seen since mid-February. Deaths per day have soared 75% in the past two weeks, climbing from an average of 244 to 426. The overall U.S. death toll stands at more than 614,000.
Across Florida, more than 12,500 patients were hospitalized with COVID-19 as of Thursday, over 2,500 of them in intensive care. The state is averaging nearly 18,000 newly confirmed infections per day, up from fewer than 2,000 a month ago. In all, Florida has recorded more than 39,100 coronavirus deaths.
Republican Gov. Ron DeSantis has taken a hard line against mask rules and other compulsory measures, saying it is important to keep Florida's economy moving.
“Florida is a free state, and we will empower our people. We will not allow Joe Biden and his bureaucratic flunkies to come in and commandeer the rights and freedoms of Floridians,” DeSantis, who has been exploring a possible bid for president in 2024, said in a fundraising email Wednesday.
The reversal in fortune at some hospitals has been stark.
In central Florida, AdventHealth hospitals had 1,350 patients hospitalized with COVID-19 as of Thursday, the most ever. The health care system has postponed non-emergency surgery and limited visitors to concentrate on treating coronavirus patients.
Less than two months ago, Miami's Baptist Hospital had fewer than 20 COVID-19 patients and was closing down coronavirus units. By Monday, hospital officials were reopening some of those units to handle an influx of more than 200 new virus patients.
“As fast as we are opening up units, they're being filled with COVID patients,” said Dr. Sergio Segarra, the hospital's chief medical officer.
In Georgia, more than two dozen hospitals said this week that they have had to turn away patients as the number of hospitalizations for COVID-19 has risen to 2,600 statewide.
Mississippi reported that its hospitals were overwhelmed with nearly 1,200 COVID-19 patients as of Thursday. State Health Officer Dr. Thomas Dobbs said the delta variant is “sweeping across Mississippi like a tsunami” with no end in sight.
In Louisiana, with roughly 2,350 coronavirus patients in hospitals, any non-emergency surgery that might require an overnight stay is being delayed at the state's largest hospital system. Dr. Robert Hart, chief medical officer at Ochsner Health, said an organ transplant involving a live donor was postponed.
“You can imagine the expectations both the recipient and the donor had leading up to the surgery, and then to have to put that off,” he said, declining to disclose the type of transplant.
The swift turn of events has been disheartening for health care workers who just weeks ago thought the battle was in its final stages. The crisis is also making it harder for hospitals to provide other crucial types of medical care.
“If you don't get vaccinated, you are taking resources from people who have diseases or injuries or illnesses,” said Dr. Vincent Shaw, a family physician in Baton Rouge, Louisiana. “COVID doesn't call people who have had strokes, who have had heart attacks, who have had other horrific or traumatic things happen and say, 'Y'all take the week off. I am going to take over the ER and the ICU.”'
In Florida, Judi Custer said she and her husband did everything they were told to do to ward off the virus. The Fort Lauderdale retirees got vaccinated and wore masks, even when the rules were lifted. Still, they fell ill with COVID-19 a few weeks ago, and 80-year-old Doug Custer was hospitalized for five days.
Judy Custer said she still believes more people need to get vaccinated.
“We've had it long enough to know it is helping people, even if they get sick with it,” she said. “You're less likely to be put on a ventilator. You're less likely to be hospitalized.”
Marcelo reported from Boston. Associated Press reporters Leah Willingham in Jackson, Mississippi; Kevin McGill and Melinda Deslatte in Louisiana; Adriana Gomez Licon and Frieda Frisaro in Miami; and Heather Hollingsworth in Mission, Kansas, contributed to this story.